0%
Ever wondered who actually has to follow those strict healthcare privacy rules you keep hearing about?
HIPAA has been the gold standard for protecting health data since 1996—but ask around, and even many healthcare professionals can’t clearly explain who the law actually applies to. Spoiler: It’s not everyone in healthcare.
If you’ve ever asked, “Does HIPAA apply to me?” or “What makes an organization a covered entity?”—you’re asking the right questions. Getting this wrong can mean building your entire compliance program on the wrong foundation.
Covered entities are the core organizations that must follow HIPAA. Identifying whether you fall into that category is the first—and arguably most important—step in any HIPAA compliance journey. Because once you're in scope, the rules are mandatory. They dictate how you handle protected health information (PHI), how you secure it, and how your vendors interact with it.
And with the 2025 HIPAA updates tightening enforcement and oversight, this is no longer just about checking a box—it’s a legal and business necessity.
So let’s start by answering the most important question: Are you a covered entity?
HIPAA covered entities are organizations that handle protected health information (PHI) electronically and transmit it for official healthcare transactions. Think of them as the gatekeepers of your medical data—they’re legally required to follow HIPAA’s strict privacy and security rules.
Here’s what most people don’t realize: not every healthcare provider is automatically a covered entity. The deciding factor is whether they conduct covered transactions electronically—things like insurance billing or eligibility checks. For example, a small family practice that only accepts cash and never submits electronic claims might not fall under HIPAA at all.
But once you're classified as a covered entity, the rules are non-negotiable. You’re required to protect patient privacy, provide individuals with specific rights over their health data, and implement administrative, physical, and technical safeguards.
And if you work with outside vendors who handle patient data? You must have formal Business Associate Agreements (BAAs) in place. These aren’t optional—they’re legal requirements.
Understanding whether you’re a covered entity isn’t just a formality. It’s the foundation of your entire HIPAA compliance strategy. Get this part wrong, and everything else could crumble.
"HIPAA compliance isn't just a regulatory checkbox—it's the foundation of trust in modern healthcare. Patients expect their data to be protected, and the cost of failure isn't just legal—it's reputational."
— David Holtzman, former privacy advisor at the U.S. Department of Health and Human Services (HHS)
Let’s break down exactly who has to follow HIPAA rules. The government actually keeps it simple: there are three types of covered entities—each with distinct responsibilities when handling your protected health information (PHI).
Not every doctor or clinic automatically falls under HIPAA. The key factor is whether they electronically transmit health information related to standard transactions like insurance billing or eligibility checks.
Who’s covered:
These are the people diagnosing and treating you, but they only become covered entities if they send your health info electronically. A cash-only practice that avoids electronic billing? They might not be subject to HIPAA at all.
Health plans are the financial engines of healthcare—they pay the bills and manage the benefits, which means they’re deeply involved in your PHI.
Covered health plans include:
Every claim, approval, and denial flows through them—and it all involves PHI.
Clearinghouses are the behind-the-scenes players that keep healthcare data flowing smoothly. They:
They’re covered entities when they perform transactions for other HIPAA-covered organizations—but depending on the setup, they may also be classified as business associates.
Understanding who’s covered is step one in HIPAA compliance.
Most people think HIPAA is just about doctors, hospitals, and insurance companies. Not quite.
Business associates are the hidden layer of healthcare—companies that handle your sensitive health data on behalf of the people you actually see. They’re not in the spotlight, but they’re just as responsible for keeping your information safe.
HIPAA doesn’t stop at the front desk. It follows your data wherever it goes—and that includes every third-party contractor behind the scenes.
Covered entities deliver care or process payments. Business associates support them behind the scenes with services that involve protected health information (PHI). Understanding the difference is key to HIPAA compliance.
Here’s how their roles compare:
| Covered Entity | Business Associate |
|---|---|
| Provides treatment, processes payments, or handles healthcare operations | Performs services or functions for a covered entity involving PHI |
| Examples: doctors, hospitals, health plans, clinics | Examples: billing services, IT vendors, legal consultants, cloud providers |
| Has a direct relationship with the patient | No direct patient relationship—works under a formal contract |
| Directly responsible for full HIPAA compliance | Must comply with HIPAA and sign a Business Associate Agreement (BAA) |
| Manages patient rights like access, correction, and consent | Assists covered entities in fulfilling patient privacy requests |
| Subject to audits, fines, and penalties for violations | Also directly liable under HIPAA and HITECH for violations |
Together, covered entities and business associates form a chain of accountability that ensures PHI is protected at every step. Whether you're delivering care or supporting it behind the scenes, the responsibility is shared—and the risks are real.
A Business Associate Agreement (BAA) is a legally binding contract between a covered entity and any third-party vendor (aka business associate) that handles protected health information (PHI) on its behalf.
It’s not just a formality—it defines what the vendor can do with PHI and holds them accountable for keeping it safe.
Every BAA must spell out that the business associate will:
Skip this step, and you're not just taking a compliance risk—you’re facing potential fines of up to $1.55 million. And under the 2025 HIPAA updates, covered entities must now collect proof that their vendors are securing data properly.
These aren’t obscure tech companies—they’re everywhere:
Here’s the twist: A covered entity can also be a business associate—depending on what it’s doing.
Examples:
If you're treating patients, you’re a covered entity. But if you’re doing back-office work for someone else’s patients, you might be a business associate in that context.
Since the HITECH Act of 2009, business associates have faced direct legal liability for HIPAA violations. And with the 2025 HIPAA updates, covered entities must now get written proof that their business associates have strong technical safeguards in place.
Bottom line: Your health data touches more hands than you think—and every one of them is responsible for protecting it.
Most people have never heard of healthcare clearinghouses. But these behind-the-scenes players handle your medical data every single day. They quietly power the billing engine of the healthcare system—and play a crucial role in keeping your information accurate and protected.
Unlike doctors or insurance companies, clearinghouses don’t deal with patients directly. But they’re still required to follow strict HIPAA regulations because of the sensitive health information they process.
Think of clearinghouses as translators or traffic controllers. They sit between healthcare providers and insurance companies, making sure the data being exchanged is clean, accurate, and in a format everyone can understand.
HIPAA defines a clearinghouse as any entity—public or private—that processes nonstandard health information into standard electronic formats. That includes billing services, repricing firms, and health data networks.
In plain terms, they take the messy, inconsistent billing data from your doctor’s office and convert it into something your insurance company’s system can actually process.
Medical billing is notoriously complex. Every provider uses different systems, and coding standards like ICD-11 have over 68,000 codes.
Clearinghouses bring order to the chaos:
They also help bridge the gap between incompatible systems and ensure the data complies with HIPAA privacy and security standards.
Nearly 80% of medical bills contain errors. Without clearinghouses, the system would grind to a halt.
Clearinghouses:
They protect both the financial health of providers and the privacy of patients. In today’s complex healthcare landscape, clearinghouses remain an essential—if invisible—part of the HIPAA compliance chain.
Think HIPAA compliance is just paperwork? Think again.
Covered entities face serious risks—up to $2.13 million per violation category per year for willful neglect (as of 2024). This isn’t about checking boxes. It’s about protecting patients and your business.
HIPAA compliance rests on five core requirements:
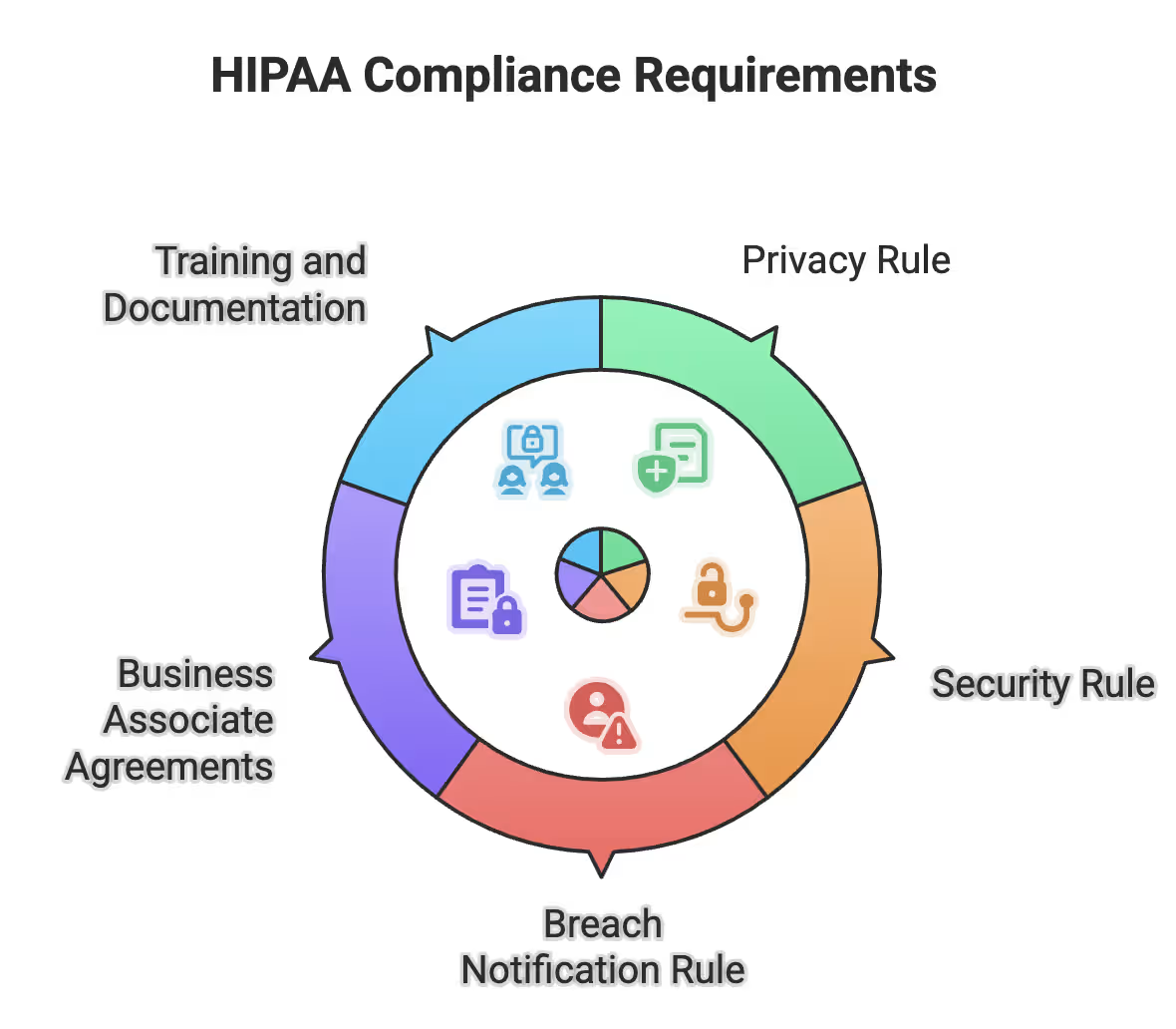
HIPAA Compliance Requirements
Let’s dive into each requirement to understand what’s expected—and what’s at stake.
This is where most organizations start—and where many fail. You must:
Every process must be documented. Every exception justified. It sounds simple, but execution is everything.
While the Privacy Rule covers all PHI, the Security Rule focuses on electronic PHI (ePHI). You need three safeguard types:
Security expectations scale with your size. A small clinic and a major hospital won’t have the same controls—but both must be effective.
When a breach happens, the countdown begins:
Your notice must include what happened, what was exposed, how patients should respond, and how to contact you.
No signed BAA? No business. Every vendor that handles PHI must:
Penalties for missing BAAs have hit $1.55 million.
Train everyone—regularly. You should:
HIPAA doesn’t specify a time, but 20–40 minutes annually per area (privacy + security) is a strong benchmark.
Missing even one of these? You’re gambling with your reputation—and millions.
The government has officially rolled out the most sweeping HIPAA changes in over a decade—and enforcement is already underway.
These 2025 updates have changed how covered entities must handle patient data, especially around reproductive health, compliance proof, and vendor oversight.
A new category—Sensitive Reproductive Health Information (SRHI)—is now under heightened protection:
No gray areas—this is a direct response to public demand for privacy. In fact, 78% of Americans support stronger protections for this data.
As of January 2025, all covered entities must actively prove compliance:
Clearinghouses and high-volume data handlers are facing increased scrutiny.
The penalty framework has been revamped:
Bottom line: Loose compliance is no longer an option. The new rules are live, audits are happening, and penalties are steep. If you haven’t updated your program yet—you’re already behind.
We’ve covered a lot, and if you’re feeling overwhelmed—you're not alone. HIPAA compliance isn’t easy. But patient privacy is serious business, and getting this wrong isn’t an option.
The numbers say it all:
The 2025 updates? They're raising the stakes—new rules on reproductive data, mandatory attestations, steeper penalties, and more audits.
Your biggest risk? Vendors. Nearly half of breaches start with third-party business associates.
So what should you do?
And here’s what most overlook: 76% of patients research your privacy practices before booking. HIPAA is no longer just about fines—it’s about trust.
Protect it—or risk losing everything.
Take control of compliance, reduce risk, and build trust with UprootSecurity — where GRC becomes the bridge between checklists and real breach prevention. → Book a demo today

Senior Security Consultant