0%
Ever wondered why data protection can feel so complicated? One moment, you’re securing information; the next, you’re buried in rules, regulations, and an alphabet soup of acronyms. Among the most frequently tossed around are PII and PHI. And here’s the catch — most people use them interchangeably. That’s not just sloppy; it’s risky.
Misclassifying these types of data isn’t a minor error. Each carries distinct regulations, protection requirements, and penalties. Get it wrong, and organizations face hefty fines, legal trouble, and, perhaps most importantly, a loss of trust from customers, patients, and stakeholders. Reputation, once damaged, is hard to rebuild.
Understanding the difference isn’t only about compliance checkboxes. It dictates how sensitive information is stored, shared, and protected across industries — from healthcare and finance to tech startups and global corporations. Handling it incorrectly can have serious financial, operational, and reputational consequences.
In this guide, we’ll cut through the confusion, clarify the key distinctions, and provide practical insights and examples. By the end, you’ll have a clear understanding of which data is what, why it matters, and how to manage it safely and effectively.
Let’s break it down clearly.
PII (Personally Identifiable Information) is any data that can identify a person directly or indirectly. Names, addresses, email IDs, Social Security numbers, driver’s licenses, or even biometric data — all fall under PII. Think of it as your digital footprint, the core of your personal identity in the data world.
PHI (Protected Health Information) is a special subset of PII. This isn’t just any personal info—it’s health-related, handled by HIPAA-covered entities. PHI includes medical records, lab results, billing information, insurance data, and any health information tied specifically to you.
The key rule: all PHI is PII, but not all PII is PHI. For PII to become PHI, it must relate to your health, healthcare services, or healthcare payments and identify you directly or indirectly.
Getting this distinction right matters. Proper classification determines which regulations apply, how data is stored and shared, and the penalties for mishandling it. Handle it correctly, and you safeguard sensitive information, maintain trust, and stay compliant across industries.
The line between PHI and PII isn’t always clear. Misclassifying data isn’t just a minor mistake — it can lead to fines, legal issues, and lost trust.
Here’s the essence: PHI is like PII’s health-focused cousin. When PII relates to health information and identifies an individual, it transforms into PHI. All PHI is PII, but not all PII becomes PHI.
| Aspect | PII | PHI |
|---|---|---|
| Definition | Any information that can identify a person (name, address, email, SSN) | Health-related information linked to an individual, handled by HIPAA-covered entities |
| Scope | Broad, across industries | Narrow, health-focused |
| Examples | Name, email, phone, SSN | Medical records, lab results, billing info, insurance data |
| Regulations | Data privacy laws (e.g., GDPR, state laws) | HIPAA, HITECH, and related healthcare regulations |
| Access Controls |
In healthcare, whether information is PII or PHI depends entirely on context, location, and usage. The same data can change categories depending on where it lives and how it’s used.
Context is king: A piece of PII in one setting can instantly become PHI when it appears in a healthcare record.
Record sets decide fate: PII stored in an Electronic Health Record (EHR) automatically transforms into PHI, triggering stricter protections.
Shape-shifting info: A spouse’s phone number may be harmless PII until added to a patient’s medical file—then it’s PHI.
Access rules are strict: PHI is only accessible to workforce members who genuinely need it for their job.
Bottom line: Correct classification ensures data is properly protected, accessed, and compliant with HIPAA regulations.
Breaches cost organizations over $50,000 on average to fix. That's not some abstract number - that's real money hitting real budgets.
Let's break down what you're actually protecting.
Healthcare organizations handle PHI in more places than most realize:
Not all PII carries the same risk, but it's all valuable to the wrong people:
The overlap between PHI, PII, and PCI creates real challenges for compliance teams. Understanding PHI PII PCI is essential to properly classify and protect sensitive information. Context is everything, and the same piece of data can fall under multiple categories depending on where it lives.
Consider this:
Sometimes a single record contains all three: health info (PHI), personal identifiers (PII), and payment details (PCI). Each has distinct rules and protection requirements.
Understanding how PHI, PII, and PCI intersect is crucial. Properly identifying and managing each type ensures compliance, reduces risk, and protects sensitive data across all systems.
The devil is in the details. And by details, we mean identifiers. You can’t just guess whether data counts as PHI or PII. There are specific triggers that determine whether personal information falls under strict healthcare regulations.
HIPAA doesn’t leave anything to chance. There are 18 identifiers that turn health information into PHI:
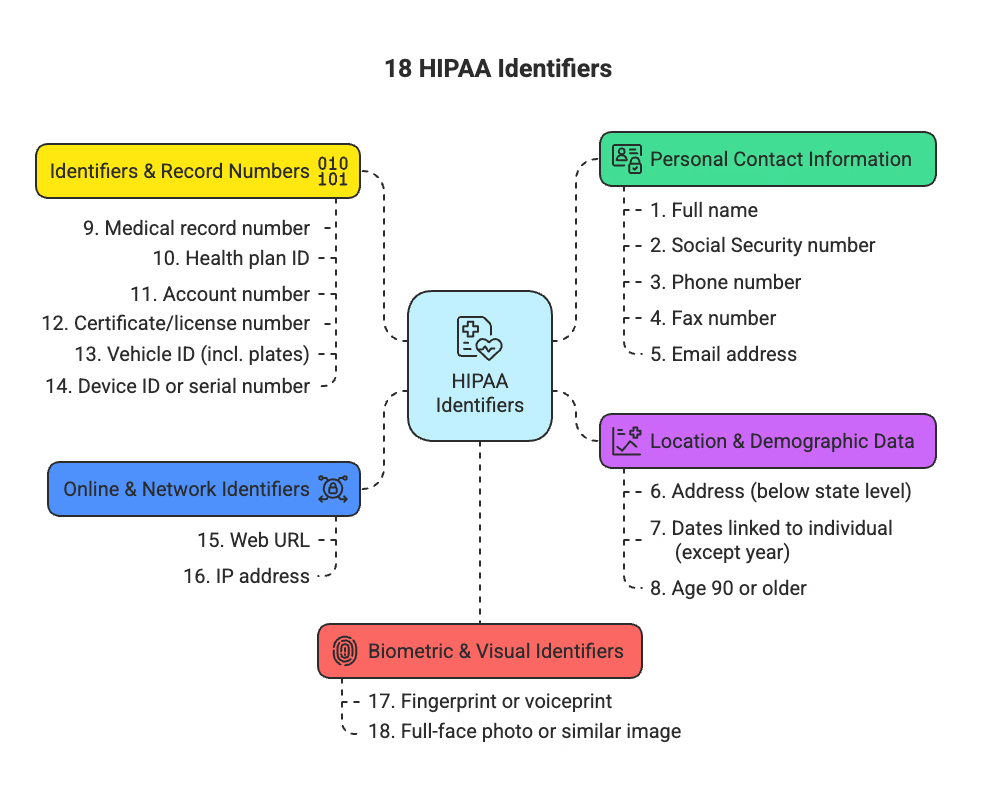
18 HIPAA Identifiers
Miss even one? That information is considered PHI.
PII follows a broader set of rules and comes in two main types:
Some PII is sensitive, such as biometric data, financial records, or login credentials. Other PII may be publicly available, like professional emails or corporate directories. The level of protection depends on sensitivity, context, and risk of misuse.
Many people overlook this: the same data can be PII in one context and PHI in another.
Healthcare context flips the switch: health records, payment for care, or any personal information stored with medical data transforms it into PHI.
The key difference often isn’t the data itself—it’s where it lives, how it’s used, and the surrounding context.
Brace yourself. The regulatory landscape for PHI and PII isn’t just complicated—it’s deliberately confusing. Multiple frameworks overlap, sometimes contradict, and create compliance headaches that keep legal teams up at night.
HIPAA sets a federal floor of protections every healthcare entity must meet:
These rules don’t just apply to hospitals and doctors. They extend to business associates—any third party handling PHI for covered entities. Miss this, and your organization is liable for the same penalties. These protections specifically apply to HIPAA personally identifiable information, ensuring sensitive health data is secured and handled according to federal standards.
NIST Special Publication 800-122 provides federal guidance for identifying and protecting PII. It helps organizations:
Think federal compliance is enough? Think again. State privacy regulations create a patchwork of requirements:
The reality? Healthcare organizations navigate both federal and state requirements simultaneously.
Welcome to regulatory chaos.
Here's a shocking truth: Only 63% of healthcare organizations currently encrypt PHI on work devices. That means 37% are walking around with unprotected sensitive data. Yikes.
Protecting PHI and PII isn't about checking compliance boxes. It's about building real security that actually works.
Encryption turns your sensitive data into gibberish for anyone who shouldn't see it:
Bonus: Encrypted PHI that gets stolen isn't even considered a notifiable breach.
Pretty powerful stuff.
Not everyone needs access to everything. Period.
Sometimes you need the insights without the personal details:
Working with third parties? BAAs aren't optional:
The bottom line? Most data breaches happen because basic protections weren't in place. Don't be part of that statistic.
Mess up PHI or PII handling? You’re staring down serious consequences. The Office for Civil Rights (OCR) has already imposed over $144 million in penalties across 152 enforcement actions—and that’s just at the federal level. Organizations can’t afford to treat this lightly.
HIPAA has a four-tier penalty system, escalating with negligence:
Yes—over $2 million per violation if rules are ignored intentionally.
Federal penalties alone aren’t enough. All 50 states have mandatory breach notification laws, with reporting timelines ranging from immediate notification to 45 days after discovery. Some recent state settlements reached $6.75 million, proving that state enforcement can be as punishing as federal action. Organizations must juggle both sets of rules simultaneously to stay compliant.
Intentional mishandling can lead to jail time:
OCR has made 2,419 criminal referrals to the Department of Justice for PHI/PII violations.
The bottom line? This isn’t just about checking compliance boxes—it’s about avoiding financial ruin, protecting your organization’s reputation, and staying out of prison.
PII and PHI aren’t just acronyms—they represent trust, responsibility, and legal obligations. All PHI is PII, but not all PII is PHI. Context is everything, and misclassifying data can be costly.
The stakes are high. HIPAA violation fines can reach $2.1 million annually for willful neglect, while OCR has issued over $144 million in penalties across 152 enforcement actions. Criminal penalties can include up to 10 years in prison and fines of $250,000 for intentional misuse.
Yet only 63% of healthcare organizations encrypt PHI on work devices. That’s more than a security gap—it’s a trust gap. A patient’s address may be PII in banking records, but in medical files, it instantly becomes PHI with HIPAA protections attached.
Compliance checkboxes aren’t enough. Encryption, access controls, de-identification, and solid BAAs are the bare minimum. Done right, data governance protects both people and your organization.
The line between PII and PHI can blur, but your commitment to safeguarding them should be crystal clear. No shortcuts. No excuses. Protect what matters most.
Take control of compliance, reduce risk, and build trust with UprootSecurity — where GRC becomes the bridge between checklists and real breach prevention.
→ Book a demo today

Senior Security Consultant
| Standard security practices |
| Strict HIPAA-compliant controls |