0%
Ever wondered why healthcare feels buried under paperwork, endless compliance checks, and nonstop regulatory updates?
Here’s the truth: risk management in healthcare isn’t what it used to be. The days of filing incident reports in dusty binders are long gone. Today, risk management is a high-stakes discipline where clinical and administrative systems must detect problems before they spiral into harm.
And the stakes? They’re staggering. Between 44,000 and 98,000 patients die every year from preventable medical errors. That’s not just another statistic—it’s families broken apart. Layer onto that the financial reality: the HHS Office of Inspector General recently reported $16.6 billion in total compliance failures. Sixteen. Point. Six. Billion.
So what exactly is at risk? Everything. Patient safety. An organization’s reputation. Financial stability and reimbursement. Market trust. Even its regulatory standing.
Healthcare risk management is no longer about plugging leaks after damage is done. It’s about anticipating risks, preventing errors, and building systems strong enough to shield hospitals from penalties, lawsuits, and tragedy.
The real question isn’t whether you should invest in risk management. It’s whether you can afford not to.
Risk management in healthcare has evolved far beyond a siloed checklist of incidents, audits, and compliance forms. In 2025, it stands as a critical discipline—reshaped into Enterprise Risk Management (ERM), where clinical quality, financial performance, patient outcomes, and organizational resilience are tightly linked.
At its core are the “great eight” risk domains: operational, clinical, strategic, financial, human capital, legal and regulatory, technology, and hazard. These domains still frame the work, but the emphasis today is sharper. Preventing medical errors, safeguarding patient privacy, securing digital systems against cyberattacks, and adapting to constant regulatory change now dominate the agenda.
The role of the healthcare risk manager has also shifted. No longer just administrators, they are communicators, trainers, and strategists. They speak with families after adverse events, coach medical teams on compliance, and design systems that prevent breakdowns before they happen. Their work directly shapes both patient safety and organizational sustainability.
The reality is clear: integrated risk management is no longer optional—it’s a business imperative. Hospitals and healthcare providers that embrace it gain stronger clinical outcomes, improved staff morale, and fewer compliance pitfalls. Those that resist? They pay in penalties, lawsuits, lost trust, and, too often, human lives.
Hospitals juggle risks on every front — from the operating room to the boardroom. One weak link can trigger a chain reaction that impacts patient safety, staff well-being, financial stability, and public trust.
While the risk landscape is broad and complex, five core domains consistently rise to the top:
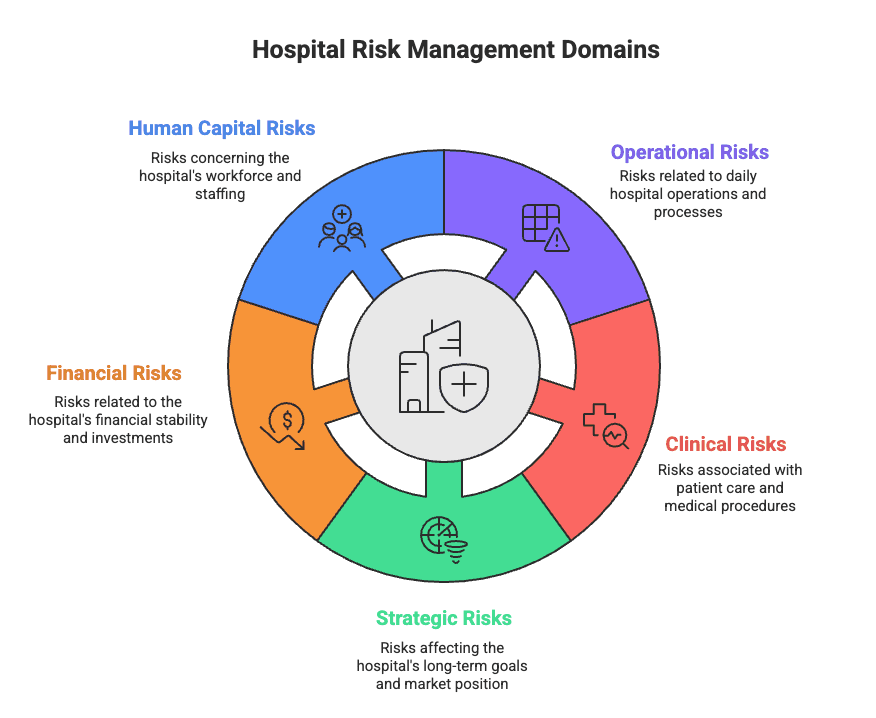
Key Domains of Risk Management for Hospitals
Each of these can disrupt care, drain finances, and erode trust if left unmanaged. Here’s how they play out in real life:
Processes, people, and systems aren’t perfect—and when they fail, patients suffer.
Operational risk assessments expose these cracks before collapse. The goal: prioritize what’s most likely to happen and what will cause the most damage.
This is where stakes are highest. Patient harm rarely comes from one error—it’s a cascade. Medication mix-ups, mislabeled specimens, or equipment failures can all prove fatal. Remember those 98,000 annual deaths from medical errors? That’s happening in hospitals right now. Clinical risk management builds defenses to catch failures before patients pay the price.
Healthcare evolves faster than most organizations can adapt. Regulations shift, payment models change, and reputations crumble if you fall behind. Strategic risk management keeps hospitals competitive while balancing compliance and care delivery.
Hospital budgets are brutal—labor eats 50–60%. Meanwhile, 768 rural hospitals are at risk of closure, with 315 in immediate danger. Malpractice verdicts regularly top $10 million, and fraud isn’t far behind: in 2023, the DOJ recovered $2.7 billion under the False Claims Act. Financial risk management is about keeping the lights on without drowning in lawsuits or fraud investigations.
Healthcare’s most valuable asset—its people—is breaking. The WHO projects a 7.2 million worker shortfall globally, with nursing demand set to hit 12.9 million by 2035. Nearly half of primary care doctors were already over 55 in 2021, signaling a looming shortage of up to 48,000 physicians by 2034. For the first time since 2008, more nurses are leaving than entering the field.
Your staff isn’t just tired—they’re done. Managing human capital risks means addressing burnout, shortages, and retention before the workforce crisis takes your hospital down with it.
Welcome to regulatory hell.
That’s not exaggeration—that’s healthcare compliance in 2025. Hospitals are buried under 629 separate regulatory requirements spread across nine domains, spending nearly $39 billion a year just to keep up. That’s money siphoned away from patient care, staff pay, and equipment—just to feed the compliance machine.
Three regulators dominate the landscape, each pulling in different directions:
Individually, they’re tough. Together, they’re chaos. Fire safety, data safeguards, and funding rules overlap and contradict, leaving hospitals trapped.
Then come state laws. Texas’ Medical Record Privacy Act outpaces HIPAA. Nineteen states already have privacy laws, with 17 more in progress. Add municipal fire codes, building codes, even noise ordinances, and compliance starts to look endless.
The real problem? Fragmentation. Nearly 47% of healthcare organizations lack centralized compliance oversight. That’s like running an orchestra where half the musicians can’t see the conductor. The cost is brutal:
The fix? Integrated GRC frameworks. HITRUST and similar models unify governance, risk, and compliance, cutting costs and reducing breaches.
Bottom line: Regulations aren’t slowing down. You either keep playing whack-a-mole—or build a system that works.
Digital transformation has painted a massive target on healthcare. Cyber threats today don’t just steal data—they can disrupt care and even put lives in danger. This isn’t a distant possibility. We’re talking about hacked life-support systems, compromised medical devices, and hospitals locked out of their own records.
Electronic health records are digital gold for cybercriminals. In April 2025 alone, the HHS Office for Civil Rights reported 66 breaches involving more than 500 records each. Compliance teams are stretched thin:
The real challenge is integration. Hospitals are forced to link dozens of systems together, often while juggling HIPAA requirements. Every connection becomes a new doorway for attackers, especially for smaller organizations without advanced defenses.
AI now supports nearly 75% of compliance teams, yet 60% admit they have no clear governance framework. Risks include:
Still, AI isn’t all downside. When properly managed, it can spot risks before they explode, flag anomalies in patient data, and automate repetitive compliance monitoring tasks.
Want an easy way to get fined? Send patient info through plain text. HIPAA penalizes unsecured communication. Secure messaging systems must include:
Forward-thinking hospitals are moving away from risky texting. Instead, they’re adopting encrypted scheduling platforms that protect PHI at every step. These systems merge security, compliance, and usability.
Today, 56% of healthcare compliance leaders rank cybersecurity as their number one headache. Without serious investment, hospitals risk more than fines—they risk patient safety.
Let’s be real—compliance risk isn’t some abstract legal concept. It’s the 3 AM spiral where you wonder if today’s the day regulators show up and ask questions you can’t answer. And in healthcare, when compliance cracks, the fallout is brutal: patients lose trust, hospitals lose money, and leadership loses sleep.
Compliance failures don’t happen by chance. They follow the same playbook:
The result? A cycle of scrambling. Over half of compliance professionals admit they’re underwater—short on staff, stretched on budgets, and missing the tech needed to keep pace.
Healthcare carries the worst breach record of any industry. In 2023, the average cost of a healthcare data breach hit $10.93 million. That’s not a statistic—it’s the price of stolen identities, leaked histories, and broken trust.
Look at the SingHealth breach: 1.5 million patient records gone. Confidential details exposed, reputations destroyed, and patients left vulnerable.
HIPAA violations cut deep:
Between 2021 and 2023, CMS issued 1,287 enforcement actions and over $4M in penalties. Most weren’t flukes. They were preventable lapses.
Audits aren’t busywork—they’re alarms. When done right, they:
Organizations using automated compliance tools spend 2.4x less time prepping audits. Translation: less scrambling, more solving.
Because here’s the truth—compliance will run proactively or reactively. One protects you. The other drains you.
Want to know what separates hospitals that thrive from those that barely hang on?
It’s not the shiny equipment or clever ad campaigns. It’s how they handle risk—every single day.
The smartest healthcare organizations don’t lock risk management in a corner office. They weave it into everything they do.
Risk management isn’t paperwork. It’s survival.
The best hospitals build risk awareness into daily workflows:
No layers of bureaucracy. No endless meetings. Just habits that catch risks before they blow up.
Here’s a stat worth underlining: healthcare organizations that use analytics for risk spotting see 47% fewer serious safety events.
Forty-seven percent.
Data isn’t just history—it’s a warning system. It can tell you:
Stop flying blind. Your data is trying to save lives—if you’ll listen.
Because they do.
Training that sticks isn’t another compliance slideshow. It’s:
Your people are both the first line of defense and the last. Train them like it matters—because it does.
Hospitals with integrated safety frameworks see 33% fewer adverse events. That’s one-third fewer patients harmed.
How? By:
Risk management isn’t a department. It’s a mindset.
When everyone owns it, patients go home healthy, staff feel supported, and the organization thrives.
When it doesn’t? You’ve already seen the numbers.
Lives are on the line. Period.
This isn’t about box-checking or dodging fines. When risk management fails, real people get hurt—98,000 preventable deaths every year. That’s not just a number. That’s families shattered.
Here’s what sets healthcare apart:
Patient safety isn’t negotiable – Bottom lines mean nothing if safety corners get cut.
Trust is fragile – IBM’s 2024 report shows 71% of patients would switch providers after a breach. That’s your patient base gone.
Financial survival depends on it – Strong compliance avoids fines and protects reimbursements.
And the inefficiency gap is real. Organizations without automated compliance waste 2.4x more time on audits—time that should go to patients, not paperwork.
Blame games don’t save lives. Clinical risk management finds causes, not culprits, and builds systems to stop tragedies before they happen.
The truth? Healthcare is complex, but those who embrace integrated risk management don’t just protect patients. They protect reputations, accreditations, and survival itself.
Because in the end, risk management isn’t red tape. It’s our best defense against the unthinkable.
Take control of compliance, reduce risk, and build trust with UprootSecurity — where GRC becomes the bridge between checklists and real breach prevention. → Book a demo today

Senior Security Consultant